Nurse practitioners (NPs) play a vital role in healthcare, especially when it comes to prescribing medications. Understanding the nurse practitioner prescribing laws by state is essential for both NPs and patients.
These laws dictate what NPs can and cannot do within their practice.
Each state has different regulations regarding prescriptive authority, which can significantly impact patient care and access to medications.
The scope of practice for NPs varies widely across the United States.
Some states allow full practice, enabling NPs to diagnose and treat without physician oversight, while others have more restrictive laws that require collaborative agreements with physicians.
This variation affects how NPs can operate and what level of care they are able to provide.
As healthcare demands increase, knowing the specific prescribing laws in your state becomes even more important for meeting patient needs effectively.
With the right information, you can better understand how NPs contribute to improving public health and enhance your interactions with these healthcare providers.
Key Takeaways
- Nurse practitioners have varying levels of prescriptive authority by state.
- Collaborative practice agreements may be required in some states.
- Awareness of these laws can enhance patient care and access to medical treatment.
Scope of Nurse Practitioner Practice
Understanding the scope of practice for nurse practitioners (NPs) is essential.
It encompasses the various responsibilities and capabilities that NPs can exercise, which vary by state.
This information helps to clarify the role of NPs in healthcare.
Defining NP Scope of Practice
The scope of practice for nurse practitioners is defined by state laws and regulations.
It includes a range of clinical activities such as diagnosing conditions, conducting assessments, ordering and interpreting diagnostic tests, and prescribing medications.
These capabilities vary widely depending on the state.
Some states allow NPs to operate independently, while others require a supervisory agreement with a physician.
In 2024, 30 states permit full practice authority, allowing NPs to perform all aspects of their training without oversight.
State Boards of Nursing and NP Practice
State Boards of Nursing play a crucial role in regulating the practice of NPs.
They set specific guidelines regarding what tasks NPs are allowed to perform.
This includes determining educational requirements and licensure processes necessary for practice.
Each state’s Board of Nursing develops rules that align with local healthcare needs.
You can check your state’s specific regulations to understand better what NPs can do in your area.
Role of the AANP in Advocating for NPs
The American Association of Nurse Practitioners (AANP) is active in advocating for nurse practitioners nationwide.
They work to influence legislation that expands NP authority and improves access to care.
AANP provides resources and support to help NPs understand their rights and responsibilities.
They also promote full practice authority in states where NPs face restrictions.
Engaging with organizations like AANP can help you stay informed about changes in NP practice laws.
Prescriptive Authority and Regulations
Understanding prescriptive authority is crucial for nurse practitioners (NPs) as it determines what medications they can prescribe and under what conditions.
This section covers key aspects of prescriptive authority, including the laws governing the prescribing of controlled substances and the specific regulations surrounding opioid prescriptions.
Understanding Prescriptive Authority
Prescriptive authority allows nurse practitioners to prescribe medications, including controlled substances.
This authority varies significantly by state.
In some states, NPs have full practice rights, meaning they can prescribe independently.
In other states, there may be restrictions, such as requiring a supervisory agreement with a physician or limiting the types of medications that can be prescribed.
Understanding these nuances is critical for NPs to avoid legal issues and provide optimal care.
To navigate these differences, refer to resources like the American Association of Nurse Practitioners.
State Laws on Controlled Substances
State laws govern how NPs prescribe controlled substances, which are categorized into schedules based on their potential for abuse.
Schedule II medications, such as opioids, have stricter regulations due to their risk of addiction.
Most states require NPs to complete a specific pharmacology course to prescribe these medications and may impose limits on how many prescriptions can be written within a certain timeframe.
The following table illustrates some common state regulations:
| State | Prescriptive Authority | Schedule II Limitations |
|---|---|---|
| California | Full | Requires collaboration agreement |
| Texas | Reduced | Limited to certain medications |
| New York | Full | Cannot prescribe more than a 30-day supply |
It’s essential to familiarize yourself with your state’s laws to ensure compliance.
Opioid Crisis and NP Prescribing Rules
The opioid crisis has led to heightened scrutiny of prescribing practices, particularly for NPs.
Many states now require additional training in pain management and opioid prescribing for NPs.
New regulations may require NPs to check prescription drug monitoring programs (PDMPs) before prescribing opioids.
These checks help identify patients who may be abusing substances or obtaining prescriptions from multiple providers.
Adhering to these updated rules is crucial for maintaining patient safety and avoiding penalties.
Always stay informed on current regulations by accessing resource sites like Medscape for the latest updates on NP prescribing laws.
Practice Authority Levels by State
Understanding nurse practitioner (NP) practice authority levels is essential for navigating the legal landscape.
States will vary in how much independence they allow NPs, influencing their ability to prescribe medications and provide care.
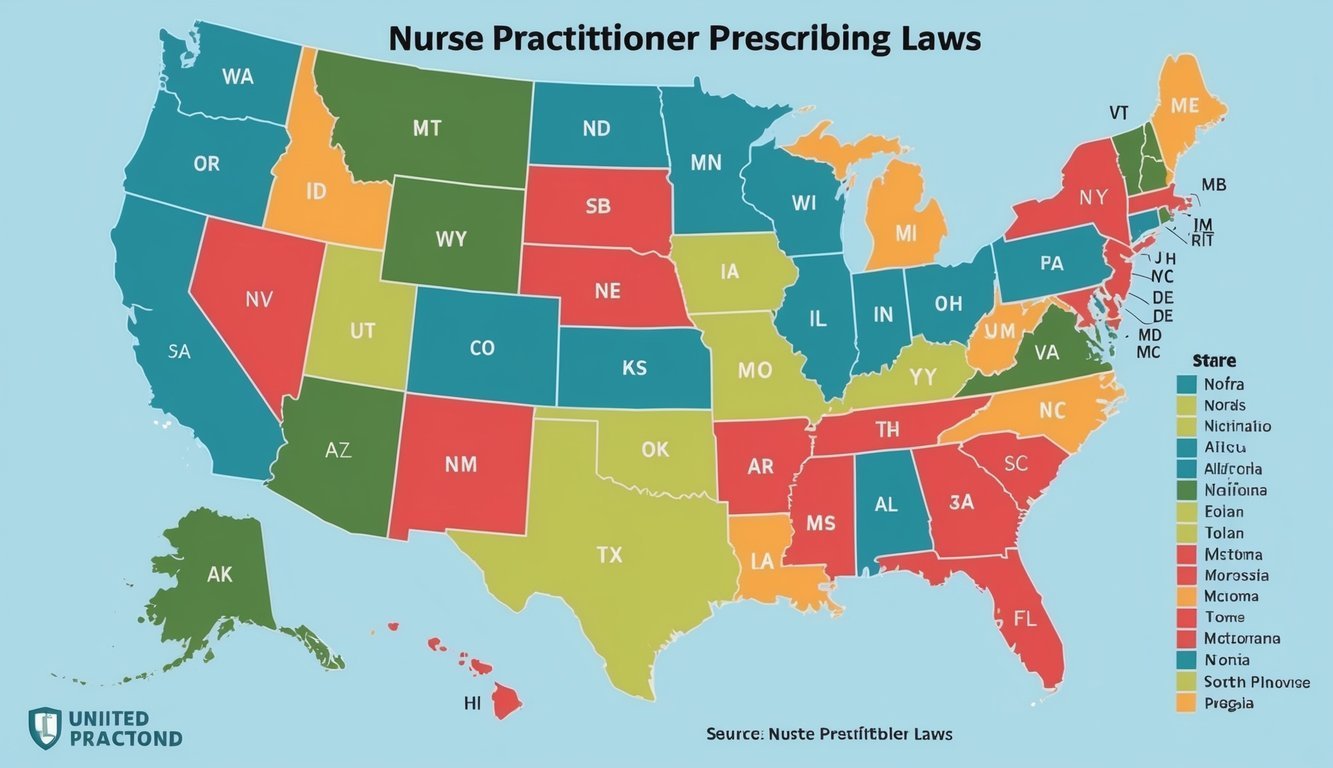
Full Practice States
In full practice states, nurse practitioners can assess patients, make diagnoses, interpret diagnostic tests, and initiate treatment plans without physician oversight.
This means NPs can prescribe medications autonomously.
As of now, states like Arizona, Oregon, and California are classified as full practice states.
In these states, the laws empower NPs to practice independently based on their education and training.
This level of authority supports NPs in providing timely care.
Full practice also addresses healthcare access, allowing NPs to fill gaps, especially in underserved areas.
Reduced Practice States
Reduced practice states require NPs to rely on physician supervision or a collaborative agreement to provide certain services, including prescribing medications.
Examples of reduced practice states include North Carolina, North Dakota, and Minnesota.
In these states, NPs must have a formal agreement with a physician, limiting their ability to act independently.
This collaborative approach can lead to increased administrative tasks, affecting the speed of care delivery.
The dynamic aims to balance patient safety with the expanding role of NPs in the healthcare system.
Restricted Practice States
Restricted practice states impose more limitations on nurse practitioners, requiring them to have physician supervision for various functions, including prescribing.
States like Texas, Virginia, and Florida fall into this category.
In these states, NPs must work closely with physicians, who have the final say in treatment decisions.
This may slow down the delivery of care and restrict the scope of services that NPs can provide.
Understanding these restrictions is crucial for NPs as they navigate their practice environment and seek to deliver quality care.
Collaborative Practice Agreements
Collaborative practice agreements (CPAs) are essential in states with specific prescribing regulations for nurse practitioners (NPs).
These agreements outline the working relationship between NPs and physicians.
Key Points of Collaborative Practice Agreements:
-
Definition: A CPA is a written contract that defines the responsibilities and scope of practice for NPs and their collaborating physicians.
-
Practice Authority: The agreement typically details the extent of the NP’s practice authority, including prescribing medications and performing procedures.
-
Physician Supervision: Some states mandate a level of physician supervision for NPs. This may include direct oversight or simply collaboration on patient care.
Requirements Vary by State
| State | Requirement for CPA | Supervision Level |
|---|---|---|
| California | Required | Varies; minimal supervision |
| Texas | Required for prescribing controlled substances | Must have supervision |
| New York | Not required, but recommended | None needed |
| Florida | Required for certain practices | Must have a supervisory role |
Boards of Nursing oversee the implementation of CPAs and ensure compliance with state laws.
They may provide guidelines to help establish these agreements.
Continuing Education and NP Competency
As a nurse practitioner (NP), ongoing education is crucial for maintaining your competency in the field.
You are required to complete a certain number of continuing education (CE) hours to keep your license.
This ensures you stay updated on best practices and new developments.
Here is a general outline of CE requirements for NPs in various states:
| State | CE Hours Required | Additional Requirements |
|---|---|---|
| California | 30 hours | 2 hours in pharmacology |
| Texas | 20 hours | None specified |
| New York | 30 hours | Must include 3 hours in infection control |
| Florida | 24 hours | 2 hours in HIV/AIDS |
These CE hours are essential for patient safety and refining your skills in evaluating patients.
As you engage in advanced practice registered nursing (APRN), you will encounter diverse cases that require up-to-date knowledge.
Staying informed through CE helps you respond effectively to clinical scenarios.
This education also strengthens your role as an NP, allowing for better patient outcomes.
By committing to continuing education, you enhance not only your own skills but also the overall quality of care provided to your patients.
Implications for Healthcare and Public Health
Nurse practitioners (NPs) play a crucial role in primary care and public health.
Their ability to prescribe medications and order diagnostic tests significantly enhances patient care.
A well-defined scope of practice allows NPs to act as primary care providers.
This ensures that patients have improved access to care, especially in underserved areas.
| Impacts | Details |
|---|---|
| Access to Care | NPs can fill gaps in services where primary care physicians are limited. |
| Patient Care | NPs manage chronic conditions and improve health outcomes through consistent monitoring. |
| Public Health | NPs support preventive care initiatives, which can lead to healthier communities. |
Nurse practice acts vary by state.
These regulations dictate how NPs can operate.
Each regulatory body establishes rules that shape NP authority in prescribing medications.
Understanding these laws is important for healthcare providers.
It helps them better navigate collaborative practices.
This teamwork maximizes the resources available to patients and ensures adherence to state regulations.
Improving NP practice authority may lead to better healthcare delivery and outcomes.
You can explore state-specific practice regulations in resources like the Nurse Practitioner Practice Authority guide.
These advancements can ultimately transform the healthcare landscape, promoting greater efficiency and accessibility.
Frequently Asked Questions
This section addresses important questions regarding nurse practitioner (NP) prescribing laws.
Understanding the scope and limitations of prescriptive authority can clarify how NPs operate in different states and the regulations they must follow.
What is the extent of prescriptive authority granted to nurse practitioners across different states?
The extent of prescriptive authority varies widely among states.
Some states allow NPs to prescribe medications independently, while others require physician oversight.
You can find detailed information on state regulations through resources like the American Association of Nurse Practitioners.
What are the limitations on medications that nurse practitioners can prescribe?
Limitations on NP prescribing often depend on the state laws.
Some states restrict NPs from prescribing certain types of medications, including specific controlled substances.
Each state has its own guidelines, which you can review for clarity.
In which states do nurse practitioners have full prescriptive authority without physician oversight?
Nurse practitioners have full prescriptive authority without physician oversight in 28 states and Washington D.C. This allows them to assess, diagnose, and treat patients independently, which may include prescribing medications.
For state-specific information, visit NurseJournal.
What are the state-specific restrictions for nurse practitioners prescribing Schedule II drugs?
Restrictions for prescribing Schedule II drugs vary by state.
Some states require NPs to have a certain amount of supervised practice or additional certifications before they can prescribe these medications.
Checking your state’s laws is essential for compliance.
Do any states prohibit nurse practitioners from prescribing certain types of controlled substances?
Yes, some states do prohibit NPs from prescribing specific controlled substances, including certain Schedule II medications.
It’s important to consult state regulations to see what substances are restricted.
How does prescriptive authority for nurse practitioners vary between restricted, reduced, and full practice states?
Prescriptive authority is categorized based on practice environments:
-
Full Practice: NPs can evaluate patients, diagnose, interpret diagnostic tests, and initiate treatment without physician oversight.
-
Reduced Practice: NPs can perform some functions but require a supervisory or collaborative agreement with a physician.
-
Restricted Practice: NPs have limited ability to engage in certain activities, including prescribing medications, often needing physician involvement.
You can explore these categories further to understand how they impact NP practice in various states.